API Publ 4743 pdf download
API Publ 4743 pdf download.Hazard Narrative for Tertiary-Butyl Alcohol (TBA)
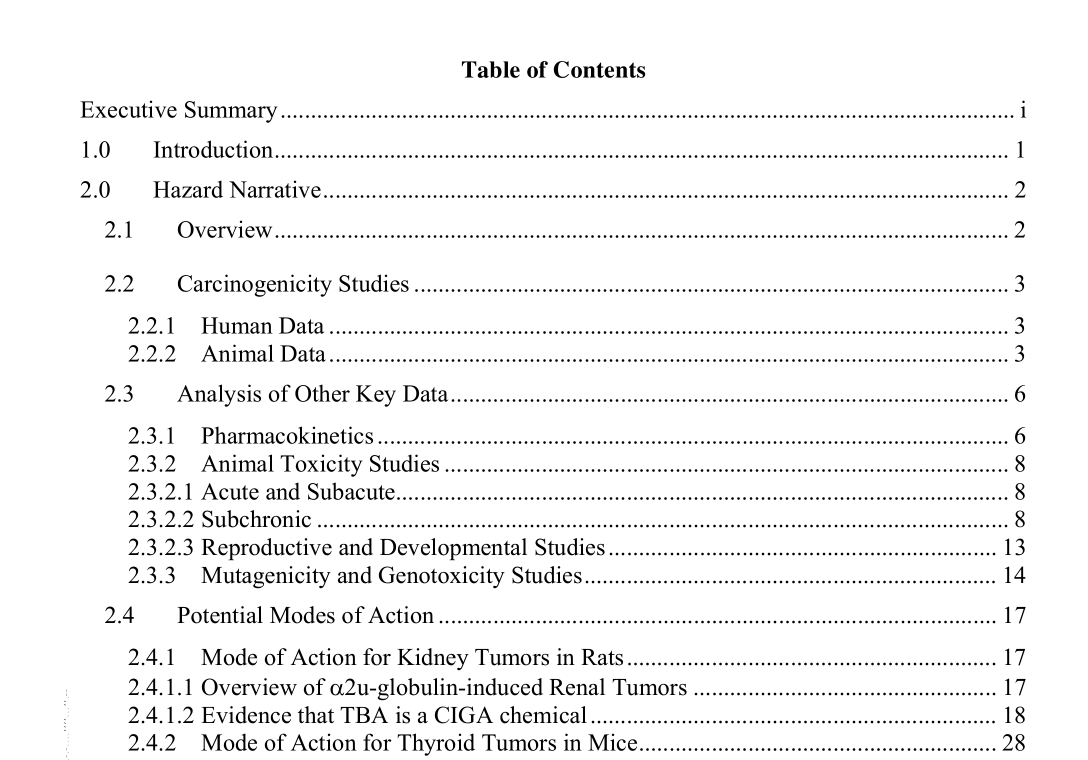
2.3 Analysis of Other Key Data
2.3.1 Pharmacokinetics Absorption of TBA from the gastrointestinal tract and distribution throughout the body occurred rapidly following administration via gavage (Faulkner and Hussain 1989; Poet et al. 1997). In female C57BL/6J mice given TBA at a concentration of 10.5 mmol/kg (777 mg/kg) via gavage every 12 hours for a total of 5 doses, TBA absorption and distribution was complete within 1.5 hours following the last dose (Faulkner and Hussain 1989). In male and female F344 rats given single intravenous dose of 0, 37.5, 75, 150, or 300 mg/kg, TBA underwent a rapid distribution phase followed by a slower elimination phase (Poet et al. 1997). Tertiary alcohols, such as TBA, are considered to be minimally metabolized via oxidative pathways (Baker et al. 1982; Thurman et al. 1980). Small amounts of acetone (ranging from 0.5% to 9.5% of the administered dose) were found in the urine and expired air of rats injected with TBA at doses ranging from 750 to 2000 mg/kg; however, the amount recovered was highly variable and did not change in a dose-related manner (Baker et al. 1982). In male rats treated with 250 mg/kg TBA via gavage, TBA was metabolized by conjugation to the TBA glucoronide and the TBA sulfate (main metabolite) and by oxidation to, 2-methyl-1,2-propanediol and 2- hydroxyisobutyrate, and small amounts of acetone (Bernauer et al. 1998).
TBA did not form aldehydes or ketones by dehydrogenation and was not a substrate for alcohol dehydrogenase (Arslanian et al. 1971; Videla et al. 1982) as it lacks the carbonyl hydrogen required for alcohol dehydrogenase activity (Baker et al. 1982). Further oxidation of 2-methyl-1,2-propanediol can result in the formation of 2-hydroxyisobutyrate, which can also be further metabolized to form acetone. In both the Bernauner et al. (1998) and the Baker et al. (1982) studies, the doses of TBA were very high (250 to 2000 mg/kg) and the resulting production of acetone in urine was very small. No differences in blood acetone levels were seen in TBA-treated male or female rats (300 mg/kg) compared to controls (Poet et al. 1997). Baker et al. (1982) could not conclude that TBA was the sole source of acetone in rat urine. In in vitro studies, TBA served as a substrate for rat mixed function oxidases (MFOs) and was demethylated to yield small amounts of formaldehyde apparently involving the interaction of TBA with hydroxy radicals generated from hydrogen peroxide (Cederbaum and Cohen 1980; 1983). Formaldehyde was not found in the urine of rats or humans following administration of TBA (Bernauer et al. 1998). Human data regarding the movement of TBA in the body are limited to results obtained from a single volunteer who ingested a gelatin capsule resulting in a dose of 5 mg TBA/kg (Bernauer et al. 1998). The major TBA metabolite in the urine of that individual was 2- hydroxyisobutyrate, with smaller amounts 2-methyl-1,2-propanediol and TBA glucuronide. In contrast to rats, only trace amounts of TBA sulfate were recovered likely due to species differences in sulfotransferase(s) (Bernauer et al. 1998). No mention was made of the presence of acetone in the urine.Elimination half-lives ranged from 3.8 hours at doses less than 300 mg/kg and were increased to 4.3 and 5 hours in the high-dose female and male rats, respectively. Poet et al. (1997) stated that the elimination of TBA appeared to saturate at higher doses. Other studies have estimated the elimination half-life to be 8 to 9 hours following oral (Thurman et al. 1980) or intraperitoneal injection (Baker et al. 1982). The doses were much higher in these studies than the doses administered by Poet et al. (1997). According to Poet et al., these doses were likely greater than metabolism/elimination saturation levels. Saturable metabolism/elimination has been reported in mice administered TBA by intraperitoneal injection at doses ranging from 5 to 20 mmoles/kg (approximately 360 to 1550 mg/kg) (Faulkner and Hussain 1989).